How to Get a Proper Shoe Fit
Many people suffer from foot problems because their shoes are poorly fitted. When shopping for a new pair of shoes, fashion usually triumphs over comfortability. A pair of well fitted shoes is essential in preventing foot problems and potential injuries.
Poorly fitted shoes can cause foot issues such as plantar fasciitis, bunions, hammertoes, ingrown toenails, and foot pain. Shoes such as high heels and sandals may cause problems for your feet. These shoes put the foot in an unnatural position for long periods and fail to provide good foot support. It is recommended to not wear either one for an extended period.
When you are trying on shoes, make sure they have enough space for your toes to move around. Shoes shouldn’t be cramped but also shouldn’t have too much room that your foot moves around in them. A snug shoe is a good choice. They should also provide good arch support and cushioning. Athletic shoes tend to offer both good support and cushioning. A degree of flexibility is necessary so they aren’t too stiff or too unsupportive.
If you can wear your shoes for a long period of time without experiencing any discomfort, this is a sign that your shoes fit properly. Do not be too dismayed if the shoe isn’t a perfect fit at first; many shoes take a few days to weeks to properly break in. However don’t expect an uncomfortable shoe to become fitted to your foot.
For those with foot conditions such as flat feet or pronation, orthotics may be helpful or even necessary to prevent foot pain. Orthotics are inserts that are placed in the shoe and provide support and cushioning for the foot. While there are many types of orthotics out there, custom-made orthotics may be necessary depending upon your foot and foot conditions.
Feet change in size over time. It is important to check your foot size over time so that you can make sure you have the perfect fit for your feet. A podiatrist can provide more information on proper shoe fitting and foot orthotics.
Three Types of Corns on the Feet

Corns are identified as patches of thickened skin and are a common foot problem that can cause discomfort and pain if left untreated. Understanding different types of corns can help in effectively managing and preventing them. Hard corns, the most prevalent type, typically develop on the tops and sides of toes or weight-bearing areas of the foot. These corns are compact and dense, often caused by friction or pressure from wearing ill-fitting shoes or repetitive motion. Conversely, soft corns tend to form between toes where sweat and moisture accumulate. These corns are softer in texture and can be more painful due to increased moisture levels. Finally, seed corns are tiny, discrete corns that often appear on the bottom of the foot. They are generally painless but can cause discomfort when walking. If you have a corn on your foot, it is suggested that you consult a podiatrist who can identify which type it is, and offer you correct treatment solutions.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Dawn Miles, DPM of Florida. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact one of our offices located in Palatka and Saint Augustine, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Understanding Corns and Calluses
Corns and Calluses are both hardened layers of thickened skin that develop because of friction. Both ailments are typically found on the feet and may be unsightly. Although they have similarities, corns and calluses are different from each other.
Some causes of corns and calluses may be wearing ill-fitting shoes and not wearing socks. If you wear tight shoes, your feet will constantly be forced to rub against the shoes, causing friction. If you fail to wear socks, you are also causing your feet to endure excess friction.
There are some signs that may help you determine whether you have one of these two conditions. The first symptom is a thick, rough area of skin. Another common symptom is a hardened, raised bump on the foot. You may also experience tenderness or pain under the skin in addition to flaky, dry, or waxy skin.
There are also risk factors that may make someone more prone to developing corns and calluses. If you are already dealing with bunions or hammertoe, you may be more vulnerable to having corns and calluses as well. Other risk factors are foot deformities such as bone spurs, which can cause constant rubbing inside the shoe.
Corns tend to be smaller than calluses and they usually have a hard center surrounded by inflamed skin. They also tend to develop on the parts of the body that don’t bear as much weight such as the tops and sides of toes. Corns may also be painful for those who have them. On the other hand, calluses are rarely painful. These tend to develop on the bottom of the feet and may vary in size and shape.
Fortunately, most people only need treatment for corns and calluses if they are experiencing discomfort. At home treatments for corns and calluses should be avoided, because they will likely lead to infection. If you have either of these ailments it is advised that you consult with your podiatrist to determine the best treatment option for you.
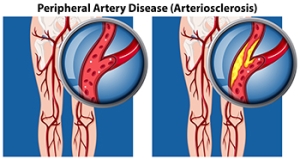
Causes and Diagnosis of Peripheral Artery Disease
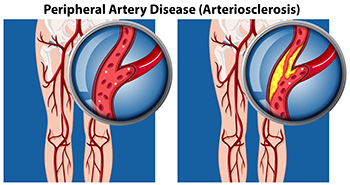
Peripheral artery disease, or PAD, poses significant challenges for foot health, stemming from restricted blood flow to the lower extremities. This condition, often caused by atherosclerosis, involves the buildup of fatty deposits in the arteries, leading to narrowed or blocked blood vessels. The diminished blood supply to the feet can result in various symptoms, including pain, cramping, numbness, and weakness, particularly during physical activity. Left untreated, PAD can contribute to serious complications such as foot ulcers, infections, and delayed wound healing. Diagnosing PAD typically involves a comprehensive evaluation by a podiatrist. This process includes a thorough medical history review, assessment of risk factors such as smoking and diabetes, and a physical examination focused on evaluating circulation in the legs and feet. Specialized diagnostic tests, such as ankle-brachial index, or ABI measurement, Doppler ultrasound, and angiography, may also be employed to confirm the diagnosis and determine the extent of arterial blockages. If you are experiencing any of the foot symptoms mentioned above, it is suggested that you consult a podiatrist who can accurately diagnose and offer relief solutions for PAD.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dawn Miles, DPM from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Palatka and Saint Augustine, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
The Importance of Diabetic Foot Care

Diabetic foot care is paramount for preserving limb health and preventing serious complications. Diabetes can lead to various foot issues, including neuropathy, microvascular disease, foot ulcers, and biomechanical changes. Neuropathy diminishes sensation, increasing the risk of unnoticed injuries, while microvascular disease impairs circulation, slowing wound healing. Foot ulcers may develop possibly leading to infections and even amputation if left untreated. Biomechanical changes further exacerbate pressure points, contributing to ulcer formation. Regular foot examinations, meticulous hygiene, proper footwear, and prompt treatment of any foot abnormalities are crucial in diabetic foot care. Podiatrists specialize in assessing diabetic foot health, providing preventive care, and offering tailored treatments to minimize complications, ensuring optimal limb preservation and overall well-being. If you have diabetes, it is strongly suggested that you include a podiatrist on your healthcare team.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dawn Miles, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact one of our offices located in Palatka and Saint Augustine, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Plantar Wart Diagnosis

Plantar warts, caused by the human papillomavirus, or HPV, are skin growths appearing on the soles of the feet, often transmitted in warm, moist environments. Though generally harmless, they can cause discomfort and resemble different problems, necessitating careful diagnosis. Treatments vary from conservative remedies to professional interventions like salicylic acid, cryotherapy, or surgery, with responses varying among individuals. Given their contagious nature, prompt treatment is advised to prevent spread. Differential diagnosis is vital to rule out more serious conditions like melanoma. Consulting a podiatrist ensures accurate identification and tailored treatment. Their expertise in foot health management, including the effective removal of plantar warts, promotes overall well-being. If you suspect plantar warts or experience foot discomfort, it is suggested that you seek professional evaluation and treatment from a podiatrist for the best outcome.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dawn Miles, DPM from Florida. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact one of our offices located in Palatka and Saint Augustine, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.